This study aimed at describing the prevalence of patients with end-stage renal disease (ESRD) receiving publicly funded dialysis in Brazil from 2008 to 2013.
In recent years, the number of patients with end-stage renal disease has rapidly increased worldwide. In Brazil, recent surveys have undisclosed a trend towards an increase in the prevalence of this condition. This study aimed at describing the prevalence of patients with end-stage renal disease (ESRD) receiving publicly funded dialysis in Brazil from 2008 to 2013. During this period there was a 25% increase in the absolute number of hemodialysis sessions (10,022,962; 12,561,623). This resulted in an estimated overall increase of 18% in the ratio of patients on hemodialysis per million population (352 pmp; 416 pmp). There were considerable differences among Brazilian States regarding the prevalence of patients with end stage renal disease on hemodialysis. In 2013, the prevalence ranged from 172 pmp (State of Amazonas) to 531 pmp (State of Minas Gerais). The leading Brazilian States, in absolute number of patients, were S?o Paulo (19,311), Minas Gerais (10,940) and Rio de Janeiro (8,510), all of them in the southeast region. In 2013, the overall mean mortality rate was 19.6%. From 2008 to 2013, the renal transplantation rate increased from 35.2 to 41.6 transplants per year per million inhabitants. In 2013, hemodialysis was the most frequent modality of therapy used, corresponding to 87.1% of the cases, followed by CAPD (9.24%) and APD (3.64%). In Brazil, chronic kidney disease is steadily increasing in prevalence and rapidly becoming a major public health concern. Therefore, policies towards its prevention and strategies to avoid underdiagnosis and assure broad access to renal replacement therapy should be nationwide strengthened.
Key words: Brazil, end-stage renal disease (ESRD), publicly funded renal replacement therapy, regional inequities, Sistema Unico de Saude (SUS)
Augusto Cesar Soares dos Santos Junior, MD PhD1,2,3
Fernando das Merc?s Lucas Junior, MD1,3
K?tia de Paula Farah, MD1,3
Ana Carolina Aguiar do Nascimento, MD1
Jos? Luiz Santos Nogueira, MD1
Carlos Faria Santos Amaral, MD1
Silvana Marcia Bruschi Kelles, MD PhD 1,2
1Nucleo de Avalia??o em Tecnologia Saude, Universidade Federal de Minas Gerais (UFMG)
2Unimed-BH, Grupo de Avalia??o de Tecnologia em Sa?de
3Nephrologist at Hospital das Clinicas – UFMG
During the past decades Brazil has undergone rapid changes in major social and economic determinants of health (1,2). Concurrently, Brazil has also experienced a rapid demographic transition resulting in an increase in the number of adults and elderly people (3). This has led to a shift in the causes of morbidity and mortality in the Brazilian population from infectious diseases to chronic non-communicable diseases (CNCD) (3,4).
In recent years, the number of patients with end-stage renal disease (ESRD) has rapidly increased worldwide resulting in a global public health problem (46). In Brazil, recent surveys have undisclosed a trend toward an increase in the prevalence of this condition (711). To face this challenge, the Brazilian public health system, Sistema ?nico de Sa?de (SUS), has increased its efforts to accomplish the State duty of providing universal coverage to all Brazilian citizens enforcing primary healthcare policies. In spite of that, Brazil still faces serious problems involving equity, quality, and efficiency of healthcare services (1,2).
In this scenario, knowledge on the prevalence of patients on chronic dialysis treatment can be decisive in the development of more effective healthcare policies (12). Therefore, this study aimed at describing the prevalence of patients with ESRD receiving publicly financed dialysis in Brazil from 2008 to 2013.
Data concerning the prevalence and mortality of patients with ESRD being provided renal replacement therapy by the SUS from 2008 to 2013 was collected at the DATASUS databank (www2.datasus.gov.br), the Authorization System for High Complexity/Cost Procedures (APAC) database, the SUS Ambulatory Information System (SIA) and the Mortality Information System (SIM) database. The absolute number of dialysis sessions was calculated considering the total number of reimbursement registries via APAC. The Brazilian government pays hemodialysis sessions on a fixed rate of 3 times per week with the possibility of an extra session every week under exceptional circumstances. Therefore, this study considered that on average one patient would undertake 150 hemodialysis sessions per year. Hence, we have estimated the absolute number of patients on hemodialysis by dividing the total annual number of sessions on a given location by 150. Other variables analyzed were region of residence in Brazil, type of renal unit (private vs. public), type of dialysis treatment (hemodialysis, peritoneal dialysis, renal transplantation) and costs. The resulting data was analyzed in September 2014.
This study produced no interventions and the privacy of the researched subjects and the confidentiality of their personal information were handled in accordance to the ethical principles of the Declaration of Helsinki.
From 2008 to 2013 there was a 25% increase in the absolute number of hemodialysis sessions (10,022,962; 12,561,623; figure 1). This resulted in an estimated overall increase of 18% in ratio of patients on hemodialysis per million population (352 pmp; 416 pmp; figure 2 and table 1). Annually, the mean increase in the number of patients was of 4,6%, figure 3.
FIGURE 1 ABSOLUTE NUMBER OF PUBLICLY FUNDED HEMODIALYSIS SESSIONS IN BRAZIL, PER YEAR
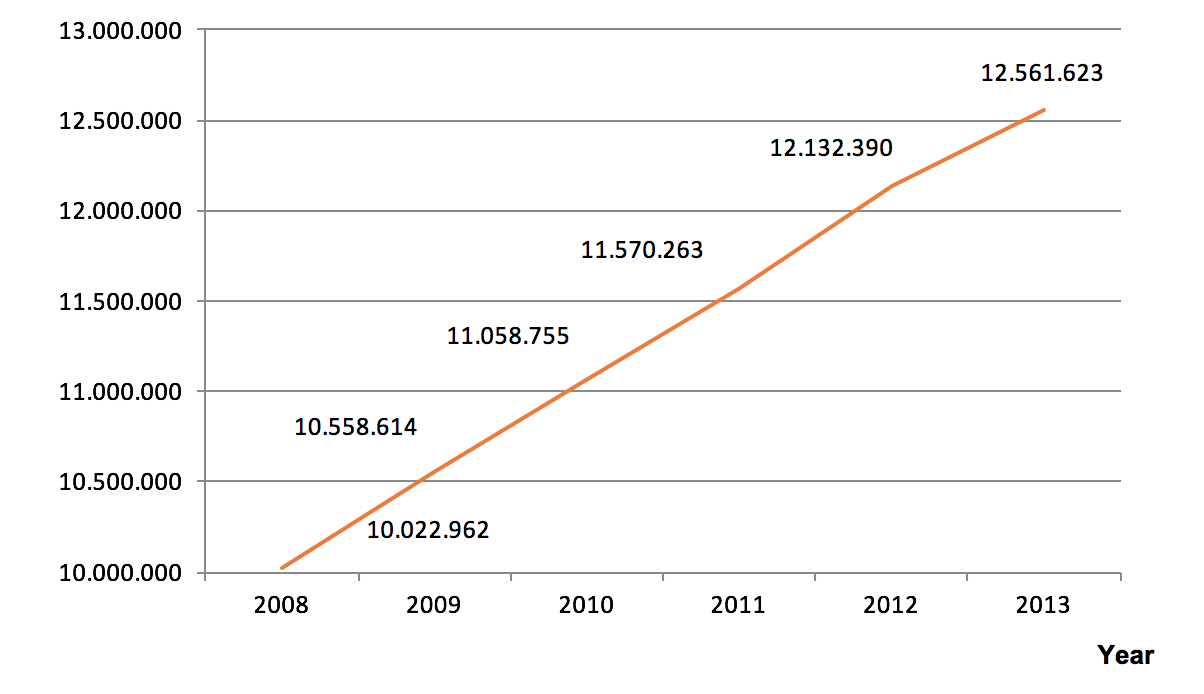
FIGURE 2 ESTIMATED ABSOLUTE NUMBER OF PATIENTS ON PUBLICLY FUNDED HEMODIALYSIS TREATMENT IN BRAZIL, PER YEAR

FIGURE 3 MEAN ANNUAL INCREASE IN THE ABSOLUTE NUMBER OF PATIENTS ON PUBLICLY FUNDED HEMODIALYSIS TREATMENT IN BRAZIL

There were considerable differences among Brazilian States regarding the prevalence of patients with ESRD on hemodialysis. In 2013, the prevalence ranged from 172 pmp (State of Amazonas) to 531 pmp (State of Minas Gerais). The leading Brazilian States, in absolute number of patients, were S?o Paulo (19,311), Minas Gerais (10,940) and Rio de Janeiro (8,510), all of them in the southeast region, figure 4.
FIGURE 4 DISTRIBUTION OF PUBLICLY FUNDED HEMODIALYSIS SESSIONS IN BRAZIL PER GEOGRAPHICAL LOCATION, IN 2013

TABLE 1 MORTALITY AMONG PATIENTS RECEIVING PUBLICLY FUNDED HEMODIALYSIS TREATMENT IN BRAZIL, IN 2013

The mean annual renal transplantation rate per million inhabitants increased from 35.2 pmp in 2008 to 41.6 pmp in 2013, figure 5 and table 1. In 2013, the overall mean mortality rate was 19.6%, table 1. In this same year, 95% of the total expenses with publicly funded dialysis sessions were allocated to treat patients on private facilities. In other words, only 5% of the expenses were spent on public dialysis facilities. In 2013, the estimated total expenses to cover dialysis and catheters costs approximated 500 million US dollars. Compared to 2008, this represented an increase of 67% in costs (R$1,344,793,917 to R$2,253,434,171).
In 2013, hemodialysis was the most frequent modality of renal replacement therapy used, corresponding to 87.1% of the cases, followed by CAPD (9.24%) and APD (3.64%), figure 6.
FIGURE 5 RENAL TRANSPLANTATION RATE PER MILLION INHABITANTS IN BRAZIL

FIGURE 6 DISTRIBUTION OF PUBLICLY FUNDED RENAL REPLACEMENT THERAPY MODALITIES IN BRAZIL, IN 2013

Currently it is believed that the underlying determinants of chronic diseases are strictly associated with the social, economic and cultural changes seen worldwide in the late decades (13). Globalization, unrestricted urbanization, population ageing, improved access to fast food and continuous exposure to unhealthy habits are some of the factors believed to have contributed to increase the burden of chronic non-communicable diseases (CNCD) especially in low and middle-income countries like Brazil (1417). In spite of that, epidemiological data regarding the burden of CNCD are still scarce. In Brazil, the Brazilian Society of Nephrology (10) regularly estimates the total number of patients on dialysis based on surveys, however this country still lacks an official public registry of ESRD patients on dialysis. Therefore this study aimed at scrutinizing databanks obtained from the Brazilian Ministry of Health focusing on the prevalence and mortality of patients with ESRD on publicly funded renal replacement therapy in Brazil.
From 2008 to 2013 there was an increase in the order of 6% in number of inhabitants in Brazil (189 million to 201 million inhabitants). In this meanwhile, in contrast, it was observed a 25% increase in the absolute number of publicly funded hemodialysis sessions in Brazil. This resulted in an estimated overall increase of 18% in the ratio of patients on hemodialysis per million population in five years (352 pmp; 416 pmp). In spite of this dramatic increase, the prevalence of patients under dialysis treatment in Brazil is still far from what is seen in developed countries as the United States, where the rate of patients on hemodialysis per million population is about 1,200 (18,19).
Considerable local differences across Brazilian States regarding the prevalence (ranging from 172 pmp to 531 pmp) and mortality (ranging from 3,4% to 32.3%) of patients with ESRD on hemodialysis was also seen. These differences suggest the existence of intrinsic regional difficulties to properly identify and treat patients with ESRD in several Brazilian regions and also raise suspicion on underdiagnose and sub notification practices. Part of these differences could also be due to economical inequities between Brazilian States once higher prevalence were specially observed in the most economic developed areas in contrast to the poorest States of Brazil.
In Brazil, only about 16% of the total dialysis sessions are provided by private funds, in spite of this, most of the current publicly funded dialysis sessions occur on private facilities (95% private versus 5% public). This suggests that the treatment of ESRD in Brazil, despite largely dependent on public funds, is critically influenced by the decisions and the quality of care provided by the private sector. This also helps to explain why despite the large territorial extension, peritoneal dialysis is the modality of choice for only about 13% of the Brazilian population under dialysis. Brazil has just taken its initial steps in establishing comprehensive policies encouraging peritoneal dialysis across the country. Therefore, Brazilian current results on peritoneal dialysis is still hugely influenced by economic and historical practices rather than a structured plan of action tailored in accordance to its population needs.
Chronic kidney disease is increasing in prevalence and therefore it is rapidly becoming a major public health concern in Brazil. Policies for its prevention and treatment should be nationwide strengthened aimed at reducing regional inequities regarding the detection of ESRD and access to renal replacement modalities across different locations in Brazil.
1. Fleury S. Brazils health-care reform: social movements and civil society. Lancet. Elsevier Ltd; 2011 May 21;377(9779):17245.
2. Uauy R. The impact of the Brazil experience in Latin America. Lancet. 2011;377(9782):19846.
3. Schmidt MI, Duncan BB, Azevedo e Silva G, Menezes AM, Monteiro CA, Barreto SM, et al. Chronic non-communicable diseases in Brazil: burden and current challenges. Lancet. Elsevier Ltd; 2011 Jun 4;377(9781):194961.
4. Rosa-Diez G, Gonzalez-Bedat M, Pecoits-Filho R, Marinovich S, Fernandez S, Lugon J, et al. Renal replacement therapy in Latin American end-stage renal disease. Clin Kidney J. 2014;7(4):4316.
5. Wagner KH, Brath H. A global view on the development of non communicable diseases. Prev Med (Baltim). Elsevier Inc.; 2012;54(SUPPL.):S3841.
6. Habib SH, Saha S. Burden of non-communicable disease: Global overview. Diabetes Metab Syndr Clin Res Rev. Diabetes India; 2010;4(1):417.
7. de Moura L, Prestes IV, Duncan BB, Thome FS, Schmidt MI. Dialysis for end stage renal disease financed through the Brazilian National Health System, 2000 to 2012. BMC Nephrol. 2014;15:111.
8. Cherchiglia ML, Machado EL, Szuster DAC, Andrade EIG, Assis Ac?rcio F De, Caiaffa WT, et al. Epidemiological profile of patients on renal replacement therapy in Brazil, 2000-2004. Rev Saude Publica. 2010;44(4):63949.
9. Oliveira De Lima A, Kesrouani S, Gomes RA, Cruz J, Mastroianni-Kirsztajn G. Population screening for chronic kidney disease: A survey involving 38 721 Brazilians. Nephrol Dial Transplant. 2012;27(SUPPL. 3).
10. Sesso RC, Lopes AA, Thom? FS, Lugon JR, Watanabe Y, Santos DR Dos. Report of the Brazilian Chronic Dialysis Census 2012. J Bras Nefrol. 2014;36(1):4853.
11. Nogueira PCK, Feltran LDS, Camargo MF, Le?o ER, Benninghoven JR, Gon?alves NZ, et al. Estimated prevalence of childhood end-stage renal disease in the state of S?o Paulo. Rev Assoc Med Bras. 2011;57(4):43641.
12. Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, et al. Priority actions for the non-communicable disease crisis. Lancet. Elsevier Ltd; 2011;377(9775):143847.
13. Alwan A, MacLean DR. A review of non-communicable disease in low- and middle-income countries. Int Health. 2009;1(1):39.
14. Hamer RA, EL Nahas AM. The burden of chronic Kidney Disease is rising rapidly worldwide. BMJ, 2006; 332:563-564.
15. Nwankwo, Bello, El Nahas M. Chronic Kidney Disease: Stemming the Global Tide. Am J Kidney Dis 2005; 45:201-208.
16. Vigitel Brasil 2011. Vigil?ncia de fatores de risco e prote??o para doen?as cr?nicas por inqu?rito telef?nico. Minist?rio da Sa?de, 2012.
17. Junior ACS dos S, Nascimento ACA. Is there an Association Between Comorbidities and Income or Literacy in Incident Dialysis Patients Living in Contagem, Brazil? Open Urol Nephrol J. 2014 Jul 24;7(1):7781.
18. U.S.Renal Data System. 2010 USRDS Annual Data Report. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2010.
19. Oliveira MB, Rom?o Jr JE, Zatz R. End-stage renal disease in Brazil: Epidemiology, prevention, and treatment. Kidney Int Suppl. 2005?;(97):82-86.
Additional Info
-
Language:
English -
Contains Audio:
No -
Content Type:
Articles -
Source:
ISN -
Year:
2015 -
Members Only:
No
